Mental health and psychosocial support (MHPSS) model
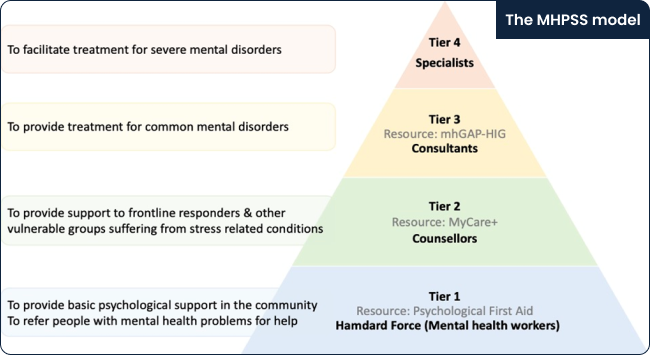
The MHPSS model is designed to address the service gaps at the community and primary health care level and help develop a pathway of care to the specialist services. The MHPSS services will be provided at four tiers:
Tier 1: Community mental health service – Hamdard Force (for basic psychosocial support)
Tier 2: Psychosocial support services (for stress-related conditions)
Tier 3: Mental health services at the primary care (for common mental health conditions)
Tier 4: Specialists services (for severe mental disorders)
Community mental health service
The objective of integrating mental health services at the level of the community in LMICs is to promote accessibility, acceptability, and scalability of mental healthcare, as well as increase the likelihood of positive clinical outcomes including treatment adherence [1] .
At the first tier, community members will be trained as a “Hamdard force” to provide basic psychological support; identify people with mental healthcare needs and refer and connect them to mental health and other relevant services. Hamdard is an adjective in Urdu meaning “empathetic”, and the title Hamdard Force describes a dual focus on the intervention and the workforce implementing it, deemed appropriate due to its cultural relevance and acceptance.
Hamdard Force will serve as a registered volunteer team and can represent frontline responders from governmental and non-governmental organizations e.g., lady health workers (LHWs), teachers, police and rescue workers; field staff of humanitarian agencies; or members of informal networks in the community e.g., community leaders, volunteer force, youth organizations, etc.
Through an intersectoral collaboration and based on an inclusion criterion, the respective departments and other agencies can nominate their staff in the field to be trained as members of the Hamdard Force. All participants will be registered on the MHPSS web portal, and after completion of a self-guided online training or a facilitated face-to-face training, they can download the Hamdard Force mobile application to connect to the MHPSS service.
The members of Hamdard Force will:
Provide basic psychosocial support
Assess individual's needs
Refer people to the MHPSS or other services
Seek supervision
Seek support for their well-being
Psychosocial support service
At the second tier, a team of clinical psychologists will provide psychosocial support services to people suffering from stress-related conditions. This team will be recruited based on pre-defined criteria in collaboration with the relevant stakeholders such as higher education institutes offering postgraduate programs in clinical psychology. After a foundational training on Tier 2 intervention - MyCare+, and being supervised by the Tier 4 specialists, the Tier 2 team will perform the following roles:
Assess, monitor, and provide psychological support to frontline responders and other individuals suffering from stress-related conditions.
Provide psychosocial interventions to cases referred by the primary care physicians (PCPs) at Tier 3, where needed.
Supervise members of the Hamdard Force
Integrating mental health services at the primary care
At the third tier, in collaboration with the respective departments of health, a team of PCPs working at the primary and secondary healthcare facilities will be selected based on pre-defined criteria. They will be trained and supervised to assess, manage common mental health conditions (by offering pharmacological and psychosocial treatments), and refer to specialists.
After training, PCPs will download the mhGAP-HIG-PK mobile application and connect with the MHPSS service to:
Assess and manage common mental health conditions at the primary care level
Refer cases appropriately (to the MHPSS service or existing specialist services).
Seek supervision on a case-to-case basis, both for urgent or routine cases.
Specialist services
Finally, at the fourth tier, experienced mental health specialists will supervise the service providers and facilitate the management and referral of difficult cases to existing psychiatric services.
The mental health specialists will be selected based on pre-defined criteria (see Annex IV), in collaboration with the relevant departments of health and academic institutes of psychiatry and psychology. The specialist resources can also be pooled to provide remote supervision, where needed. They will be trained as trainers (on mhGAP-HIG guidelines) to:
Train and supervise teams at tiers 2 and 3
Provide brief online consultations to the referred cases, where needed.
Facilitate referral pathways to existing services.
THE MHPSS SERVICE MODEL
The MHPSS model is structured into four interconnected tiers for delivering MHPSS service in Pakistan, to integrate mental health care at the level of community and primary care, to increase access to care for people suffering from mental health conditions, and to strengthen existing services at the level of districts and tertiary care. Based on the level of intervention required, the four-tiered system helps to delegate the responsibility of providing care (commonly known as task sharing) to a newly trained mental health workforce.
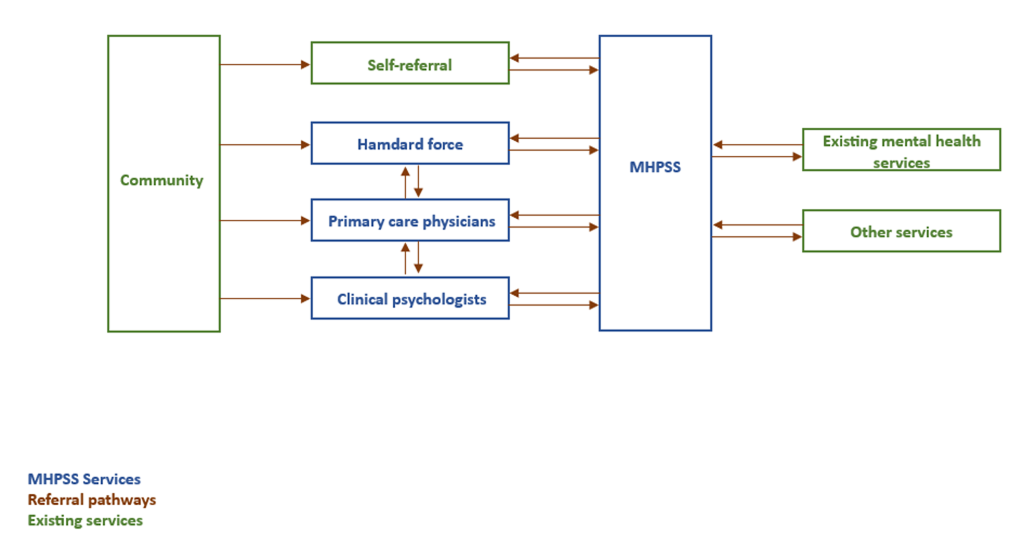
The MHPSS service model helps to ensure that people experiencing mental distress can seek help, even in areas with inadequate internet connectivity or limited use of mobile phones. This can be achieved by reaching out to the trained members of Hamdard Force, or by making an appointment through the MHPSS web portal or a dedicated phone service.
The MHPSS response team will reach out to the referred person within three working days (for routine cases) or one working day for urgent cases. After evaluating the level of intervention needed, the response team may recommend self or guided help through the MyCare+ mobile application. For cases suffering from common mental disorders, they will be referred to the nearest trained PCPs and those suffering from severe mental disorders will be referred to the specialists at Tier 4 or to the existing services, as needed.
The PCPs can also refer people suffering from severe mental disorders to the specialists at Tier 4 or the existing services, as needed. They can also refer people to the clinical psychologists at Tier 2 for stress-related conditions if required.
At Tier 4, specialists guide the management of difficult cases or refer these to the relevant services. The model can help develop an effective (internal and external) referral mechanism connecting all tiers (internal) and with relevant existing services (external). This approach has the potential to enhance accessibility and continuity of care, thus reducing the treatment gap and providing effective and responsive mental health services.
MHPSS model is rights-based and person centred?
The MHPSS model is unique with its rights-based and inclusive approach and was launched to address numerous existing challenges. The foremost challenge is that mental health services are available in urban clusters only and are not easily accessible for the vast majority who have to travel long distances to see a specialist, face long waiting hours in specialists OPDs/private clinics, and bear out-of-pocket expenses. The existing services are not just bio-medical in approach, with little emphasis on providing psychosocial care, but focus on specialists’ care, thereby not cost-effective to scale up. Most of these services are limited to clinical settings in tertiary care hospitals and do not address the needs of people in the community or complex needs that emerge after any humanitarian crisis (e.g., the COVID-19 pandemic, floods, terrorism, etc.). Lastly, not all available services follow evidence-based practices or are well-regulated.
The MHPSS model aims to address these challenges and protect the rights of people living with mental health conditions as follows:
Using digital technology, the MHPSS services are designed to be easily accessible, offering both digital and in-person access to the service users.
These services are evidence-based, and person-centered; protect the privacy of service users and their data; and are regularly monitored to ensure transparency and encourage accountability by seeking regular feedback from service providers and users.
In order to scale up services, the model utilizes the task-sharing approach where tasks needing lesser expertise are assigned to a workforce with supervision from highly trained personnel. This workforce is selected through pre-defined criteria and includes equal representation from both genders and people with lived experience, where possible.
All training resources are evidence-based, developed on principles of rights-based care and contextualized to local needs
Scientific protocols have been developed for assessment and therapeutic interventions and regular supervision will be provided to implement these interventions.
The model will be implemented through intersectoral collaboration with relevant stakeholders to address the emerging mental health and psychosocial challenges in humanitarian settings, faced by the vulnerable population and frontline responders.
It also integrates cross-cutting themes like gender, climate change, human rights, and cultural sensitivity into its framework to ensure equitable and accessible mental health services in humanitarian settings.
It promotes community resilience and traditional coping mechanisms. Contextualized evidence-based interventions and collaboration with community leaders and people with lived experiences have been adopted to address the stigma associated with mental illness and encourage professional help-seeking.
The model offers a safe space for women facing gender-based violence where they receive non-coercive service while ensuring their confidentiality and consent. The training of the workforce employs gender-sensitive and trauma-informed practices to ensure sensitized support to vulnerable groups.
Mental Health Strategic Planning & Coordination Unit Health Section Ministry of Planning, Development & Special Initiatives